Assessing Dose Administration of Lu-177 Dotatate Therapy: Quantifying the Residual Dose, Second Instalment
Résumé
Au cours d’une radiothérapie, le dotatate marqué au Lu-177 est typiquement dilué dans une poche de sérum physiologique, puis infusé chez le patient par intraveineuse. Une fois administrées, la poche de sérum physiologique et l’intraveineuse sont rincées pour s’assurer que la dose résiduelle soit administrée au patient. Toutefois, changer le sac de perfusion dans une seconde poche de sérum physiologique augmente le risque de contamination. Christian Detlef Raharja voulait savoir si le fait de rincer l’intraveineuse après la radiothérapie au Lu-177 améliore l’administration d’une dose ou si le fait de jeter l’intraveineuse et la poche de sérum physiologique constituerait une meilleure pratique.
Cet article sera présenté en trois segments. Dans le premier segment, l’auteur décrivait sa question et son hypothèse de recherche. Dans ce deuxième segment, il en décrit les procédures et évaluations. Enfin, le segment final discutera des résultats de sa recherche.
by Christian Detlef Raharja
With contributions by Edward Sun, Judy Gabrys, and Rebecca Wong
The Michener Institute, University of Toronto
Background
When conducting Lu-177 therapy, the Lu-177 dotatate is typically diluted in a saline bag and then infused through an intravenous (IV) line to the patient. After administration, the saline bag and IV line are flushed to ensure the residual dose is administered to the patient. However, changing the infused bag to the second saline bag increases the risk of contamination. The author wanted to know if flushing the line after Lu-177 therapy improves dose administration or if discarding the line and saline bag would lead to better practice.
This paper is presented in three instalments. In the first instalment, the author described his research question and hypothesis. In this instalment, he will describe the procedures and evaluations.
Methods
Study population
This sub-study was conducted at the Princess Margaret Cancer Centre in Toronto, ON, with post-Ga-68-dotatate patients positive for neuroendocrine tumours (NETs). The patients’ workup prior to therapy is shown in Figure 3.

Figure 3: Patient’s work-up prior to Lu-177-dotatate therapy.[1]
The six-month study involved 15 patients and 25 cases (some patients had multiple trials). There were no age or gender restrictions for the therapy itself. Following are the inclusion and exclusion criteria for Lu-177 therapies.
Table 1: Inclusion and exclusion criteria for Lu-177 therapies.[2]
| Inclusion Criteria | Exclusion Criteria |
|
|

Figure 4: Packaging of the infusion set used within the study.
Procedure
Materials needed:
- Lu-177 dotatate dose (approximately 7.4 GBq (± 10%) infused in a 100 mL saline bag)
- IV line
- saline bag (used after Lu-177 administration to flush the line)
- second IV line (used to cap the patient’s line)
- dose calibrator
- 20 mL syringe with a 21-gauge needle (used to draw up the excess saline from the bag as well as the Lu-177 dotatate dose from the vial)
- radioprotective container (used to transport the dose to prevent further contamination)
- Geiger-Mueller pancake probe (used to ensure there was no contamination on the radioprotective Lu-177-dotatate protective container that the dose was in when it arrived and to monitor the area post-administration)
The Lu-177 dotatate vial was assayed to ensure there was sufficient activity to draw up. The dose ordered[3] was drawn with a syringe and assayed. The same volume of saline as the dose was removed from the 100 mL saline bag with a syringe. The dose was then infused in the saline bag and placed in a radioprotective container to be transferred to the inpatient unit.
After the patient had been greeted, a radioactive warning sign was placed on the patient’s door and the infused saline bag was placed on the patient’s IV pole. The infusion pump was set to 200 mL/hr and the Lu-177 dotatate was infused over 30 minutes.[4]
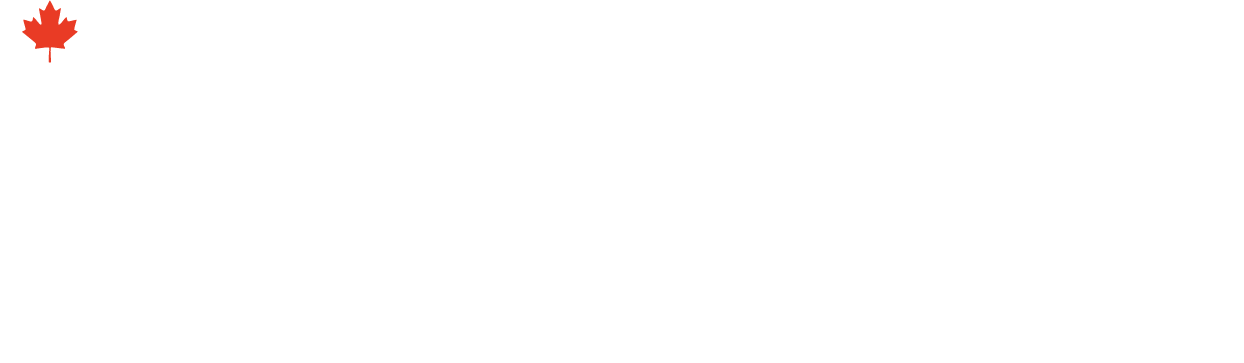
A volume scale was used to estimate the volume in the line (shown in Figures 5 and 6).

Figure 5: Volume within the chamber and IV line of the infusion set.

Figure 6: The 17 mL chamber divided into quarters to approximate the corresponding volume of the quarters.
After administration of the Lu-177 dotatate, a photograph was taken of the chamber and compared qualitatively to the chamber with saline injected at different marked points (shown in Figure 7). This approximated the volume of residual dose left within the chamber and line. The average of each volume was calculated to see the significance of volume compared to residual dose activity.
Figure 7: Examples of the chamber volumes from patients. (Note: Varying camera angles limited the ability to quantify the chamber volumes. Keeping camera angles consistent going forward will reduce variability.)
After the Lu-177 dotatate was administered and pictures of the IV line and chamber were taken, the saline bag and IV line were capped and carried in a radioprotective container to the PET radiopharmacy, where the dose calibrator was located.
The bag and line were assayed separately and the data recorded. This extra step of assaying the bag and line was not part of the standard protocol.
The decay, which was insignificant since the half-life of Lu-177 dotatate is 6.64 days,[5] was not accounted for.
After being assayed and recorded, the IV line was brought back up to the inpatient unit in the radioprotective container. The IV line was then flushed aseptically with a 25 mL saline bag at 300 mL/hr.[6] The line was assayed again to check for error during flushing. The extra time required to flush the line was also measured using a stopwatch.
The data was recorded in an Excel spreadsheet and compared to see what percentage of the actual dose was lost through the residual dose prior to flushing. This data was recorded weekly and the statistical significance was expressed as mean ± standard deviation as well as through a one-tailed Z-test.
The volume of residual dose in the chamber and IV line was accounted for and recorded and was analyzed for statistical significance through a Pearson correlation coefficient test.
Evaluation instruments:
- Consent form (acknowledging the procedure and risks involved)
- Dose calibrator (used to assay Lu-177 dotatate vial and dose pre-administration and the IV line and saline bag post-administration)
- Microsoft Excel (used to record data and check for significance)
- Geiger-Mueller pancake probe (used to check for contamination)
- Camera (used to take pictures of the IV line chamber)
- IV chamber scale (used to approximate the volume of the IV chamber through qualitatively comparing with the photos taken)
- Stopwatch (used to measured the extra time allocated for the project)
Data analysis
The statistical significance of the residual dose was analyzed using a Z-test, which calculates the probability of the measured activity occurring within our normal distribution. Specifically, an upper-tailed test of population mean with known variance was used. Making the null hypothesis (H0) that there was 10% of the Lu-177 dotatate dose or more residual activity within the IV line, we wanted to determine if we could reject this null hypothesis at a 0.05 significance level (p < 0.05).
A bivariate Pearson correlation coefficient test measured for statistical evidence of a linear relationship between the volume of the chamber and IV line compared to the activity measured. Specifically, a one-tailed significance test was used to see if there was no association (r = 0), a positive correlation (r > 0), or a negative correlation (r < 0) where r was the population correlation coefficient. A p-value (p < 0.05) would then be extracted from this r-value.
Ethical considerations
This project, being a sub-study of the Lu-177 dotatate trial, did not need the approval of the Research Ethics Board; the research trial had already been approved and there were no added risks to the patients. Before therapy, patients had to sign a consent form, which ensured they understood the risks and benefits involved with this procedure and the exact steps of the therapy.
Benefits of this project:
- Treating the NETs discovered through a Ga-68-dotatate scan
- Developing a more accurate assessment of dose administration, which would create better practice for the technologist and a definitive approach to the administration of Lu-177 dotatate
- Answering the question of whether flushing was a necessary process when administering the dose
There were no clear risks that would cause harm to the patient within this quality assurance project, but the patient may have experienced stress caused by the additional time necessary to assay the residual activity during the administration of Lu-177 dotatate. The risk of exposure to the patient’s kidneys was explained so that the patient understood potential negative outcomes from this trial.
The patient was informed that any information obtained within this study was confidential. If their data was used in the study, the patient was assigned a reference number to ensure their anonymity. Any data written on paper was kept by the primary researcher and away from the public eye. Electronic data was stored safely on a computer and was only accessed by the researchers involved in the study.
There was potential risk to the technologist carrying the Lu-177 dotatate between the PET radiopharmacy and the inpatient unit. This step was not part of the standard protocol and increased the risk of contamination to the technologist as they spent more time handling the Lu-177 dotatate than normal.
References
1. Wong, R., 2015. A prospective phase II, single-arm, multi-centre, study of the efficacy and safety of lutetium-177 octreotate (Lu- dotatate) treatment in patients with somatostatin receptor positive neuroendocrine tumours. Ozmosis Research Inc., 1, 1–56.
2. Ibid.
3. The activity of the dose was ordered from the radiation oncologist.
4. The standard protocol used for Lu-177 dotatate administration was created by Ozmosis Research Inc.
5. Stavrou, P.Z., et al., 2016. Residual activities of 99mTc-labelled radiopharmaceuticals in routine nuclear medicine practice. Nuclear Medicine Communications, 37(6), 658–663.
6. As per the protocol defined by Ozmosis Research Inc.
 Christian Detlef Raharja
Christian Detlef Raharja
Christian Raharja is a nuclear medicine student at the Michener Institute, University of Toronto. His current clinical rotation is within the University Health Network, which includes Toronto General Hospital, Toronto Western Hospital, and SickKids Hospital. His work focuses on creating quality assurance projects to improve the current trials and procedures implemented in the hospitals he works in. His hobbies include weightlifting, cooking, paddling (dragon boat), and travelling.
Christian Raharja étudie présentement la médecine nucléaire à l’Institut Michener de l’Université de Toronto. Il effectue présentement son stage clinique au sein du réseau de santé University Health Network, qui inclut le Toronto General Hospital, le Toronto Western Hospital et le SickKids Hospital. Ses recherches sont centrées sur la création de projets d’assurance qualité afin d’améliorer les essais et procédures actuels mis en circuit dans les hôpitaux où elle travaille. L’haltérophilie, la cuisine, le bateau-dragon et les voyages font partie de ses principaux passe-temps.

 Christian Detlef Raharja
Christian Detlef Raharja