President’s Message, June 2020
 The philosopher Roger Bacon (1214–1292) once stated, “There are many dense bodies which altogether interfere with the visual and other senses of man, so that rays cannot pass with such energy as to produce an effect on the human sense and, yet nevertheless rays do really pass through without our being aware of it” (Bridges, 1897).
The philosopher Roger Bacon (1214–1292) once stated, “There are many dense bodies which altogether interfere with the visual and other senses of man, so that rays cannot pass with such energy as to produce an effect on the human sense and, yet nevertheless rays do really pass through without our being aware of it” (Bridges, 1897).
Although Bacon was largely referring to more sensory perceptions of light, sound, and heat, it’s clear that, as long ago as medieval times, some academics understood that not all that exists in the ether[1] could be easily explained, but there could be “cause and effect” for exposure. Since the concepts of radiation protection deal largely with cause and effect, I decided to spend this Bulletin message exploring some early history of radiation protection (with the caveat that we cannot cover it all here!).
 |
An early X-ray procedure.
File: Early x-ray procedure.jpg. Downloaded from Wikimedia. Description: Photo of an early X-ray procedure, using a fluoroscope screen, around 1910. No precautions to minimize exposure were taken since the dangers of x-rays were not known at the time. The caption read: ‘A physician examining the bones of the arm by means of X-rays’. Original source: Burns, Elmer Ellsworth. (1910). The Story of Great Inventions, p. 233, fig. 117. New York: Harper & Brother. Permissions: Public domain. |
Early history of radiation protection
In December 1895, Wilhelm Conrad Röntgen (Germany) discovered X-rays, and in November 1896, Henri Becquerel (France) discovered radioactivity in uranium. Émil Herman Grubbé (US), a manufacturer of Crookes tubes[2] in Chicago, was using his equipment to study the fluorescence of materials as early as 1896. In January of that year, Grubbé noticed that he had developed hand erythema, ulceration, and scarring. Noting the possible therapeutic aspects of X-rays, Grubbé treated a patient with breast cancer at the end of January 1896 (Grubbé, 1933).
John Daniel and William Lofland Dudley at Vanderbilt University (US) radiographed Dudley’s head in February 1896 and produced the first diagnostic X-ray (Sansare et al., 2011). In July 1896, Victor Despeignes (France) reported using X-ray to treat stomach cancer (Leszczynski & Boyko, 1997).
In March 1897, Stone Scott (US) reported on 69 cases of skin damage due to X-ray (Scott, 1897). And, of note, the first lawsuit for radiation burns was filed in 1899 (Grand Forks, 1899).
While Bergonié and Tribondeau (France) were studying cellular changes in rat testicles due to X-ray exposure in 1904 (Vogin & Foray, 2012), Heineke (Germany) was producing leukemia in rats from X-ray exposure in 1903 (Heineke, 1905).
It’s clear that, within the first decade after the discovery of X-ray and radioactivity, a lot was going on worldwide to study the effects of ionizing radiation exposure.
In Germany around 1911, Otto Hesse collected histories of 94 cases of radiation-induced tumours (50 cases among early radiologists) (Hesse, 1911). In 1922, René Ledoux-Lebard (France) estimated that more than 100 early radiologists had died of occupationally induced cancer (Patterson & Thomas, 1973).
The first reported death of a female worker in the radium dial industry was in 1925 (Rowland, 1994). In 1939, Sigismund Peller (US) reported 47 lung cancer cases from 400 miners in the Joachimsthal pitchblende[3] mines in Bohemia (NRC, 1988). Indeed, the science of epidemiology, which was introduced in the mid-1800s for infectious diseases, began to be used to study exposure to non-infectious agents, such as radiation exposure.
Formalization of radiation protection regulations was starting within about 15 years of the discovery of X-rays! The German Radiological Society set standards in 1913 based on skin erythema doses (Stabin, 2007). In 1915, the British Roentgen Society started making radiation safety recommendations (Meinhold, 2004). Many places set their own standards based on measured skin erythema doses for their equipment (300–600 rads, typically) (Inkret, et al. 1995).
The British Society’s X-ray and Radium Protection Standards Committee was formed in 1921 and published recommendations between 1921 and 1948 as additional knowledge was gained regarding radiation safety. For example, the 1921 British Protection Standards recommended:
(i) No more than seven working hours per day,
(ii) Sundays and two half-days off per week,
(iii) As much leisure time as possible spent out of doors,
(iv) Annual holiday of one month or two fortnights, and
(v) Sisters and nurses, employed as full-time workers in X-ray and radium departments, should not be called upon for any other hospital service. (Meinhold, 2004)
Arthur Mutscheller (US) established the first quantitative tolerance dose limits in the mid-1920s. He set a limit of 1/100th of the skin erythema dose in a 30-day period, corresponding to a dose of 72 rads per year (Inkret et al., 1995). Early radiologists received 50 rads per year (500 mGy per year) on average. Compare that with the current Canadian Nuclear Safety Commission (CNSC) maximum worker limit of 50 mSv in a given year, with no more than 100 mSv over a five-year reporting period.[4]
The United States created the Advisory Committee on X-ray and Radium Protection (ACXRP) in 1929, and their first recommendations in 1931 suggested a limit of 0.2 R per day[5] (50 rads per year), being reduced in 1936 to 0.1 R per day (25 rads per year) (Stabin, 2007).
To aid in quantifying exposure, film badges and ionization chambers were developed in the 1920s. Robert Landauer (US) used dental film with filters to estimate skin erythema tolerance limits, and Victoreen manufactured its first Condenser R-Meter in 1923, permitting quantitative radiation measurements to be made (Taylor, 1981).
In 1941, ACXRP established the maximum permissible body burden (MPBB) for radium at 0.1 µCi (0.1 µg) (Rowland, 1994).
The first nuclear reactor (the Chicago Pile) was constructed at the University of Chicago and tested on December 2, 1942, and the field of modern health physics began. (The term “health physics” was proposed to conceal the fact, during wartime, that this was the science of radiation protection.)[6] The National Council on Radiation Protection and Measurements (NCRP) was formed out of the ACXRP in 1946 (Stabin, 2007). Meanwhile, in Canada, the Atomic Energy Control Board (AECB) was established in 1946 and became the CNSC[7] in 2000. To bring this full circle, in 1979 the Canadian Radiation Protection Association (CRPA) was formed!
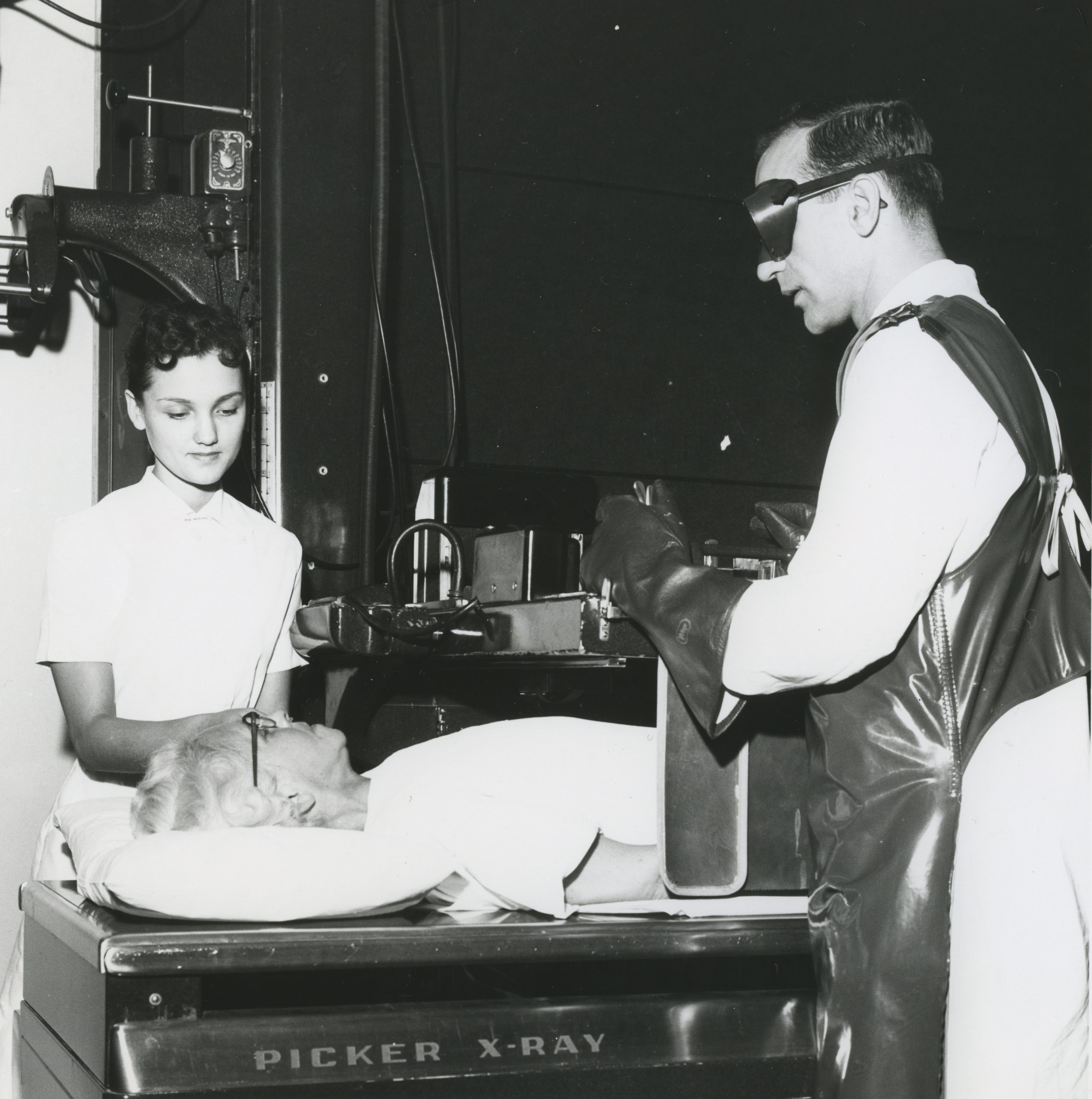 |
X-ray at St. Joseph’s Hospital in Sarnia, Ontario, 1946.
File: Picker x-ray machine (16087410301).jpg. Downloaded from Wikimedia. Description: X Ray in progress, St. Joseph’s Hospital, Sarnia. Original source: Flickr. Author: Congregation of Sisters of St. Joseph in Canada. Date: 1946. Permissions: This image was taken from Flickr’s The Commons. The image license was automatically confirmed using the Flickr API. |
Why is the early history of radiation protection important?
I think it’s important to acknowledge the scientific investigation of, and often pain and suffering endured by, early pioneers in the practice of radiation protection. In Canada, we now have well-developed radiation protection regulations, consistent with international best practices, developed on the backs of leading pioneers in the field.
CRPA is proud to be a radiation safety organization with goals to
- facilitate member exchange of scientific and technical information,
- publish findings,
- promote education and professional development,
- aid in developing guidance and standards, and
- support the activities of other safety-focused organizations.
We remain together, whether it be face-to-face or physically distanced, to advocate for radiation safety in Canada and abroad.
Be safe!
 |
An early fluoroscope screen.
File: American X-ray journal (1902) (14570925627).jpg. Downloaded from Wikimedia. Original source: O’Hara, Dr. Fred S. (1902). X-Ray Narrative. American X-Ray Journal, 11(1), p. 1083. Permissions: This image was taken from Flickr’s The Commons. |
Notes
1. The ether: the upper regions of the sky beyond the clouds.
2. An experimental electrical discharge tube (with partial vacuum) invented by English physicist William Crookes in the late 1800s.
3. Pitchblende, a uranium-rich byproduct of silver mining, was once used in yellow and orange dyes. (For more, see Mining’s Bohemian boomtown, Canadian Institute of Mining, Metallurgy and Petroleum [CIM])
4. See Radiation Protection Regulations (SOR/2000-203).
5 . Roentgen (R) is a historical exposure unit first derived for quantifying X-ray exposure. One roentgen (1 R) is equal to the amount of charge generated in a cubic centimetre of air and can be shown equivalent to 0.877 rad in air, or 0.95 rad in tissue. For photons, 1 roentgen is approximately equal to 1 REM (or 10 mSv). Caution: since 1 roentgen ~ 1 REM, it is not uncommon for R to have multiple potential meanings!
6. See Why did they call it that? The origin of Selected Radiological and Nuclear Terms.
7. See “Canada’s Nuclear History.”
References
Bridges, K. (1897). The “Opus Majus” of Roger Bacon, Vol. 1. Oxford, UK: Oxford Press.
Grand Forks. (1899, April 6). “Burned by Roentgen Rays,” Grand Forks Daily Herald, p. 7.
Grubbé, E. H. (1933, August). “Who Was the First to Make Use of the Therapeutic Qualities of the X-ray?” Radiological Review XXII, pp. 184–187.
Heineke, H. (1905). “Experimental Investigation of the Effect of Roentgen Rays on Bone Marrow and Roentgen Treatment of Leukemia, Pseudoleukemia and Sarcomas,” Deutsche Zeitschrift für Chirurgie, 78, p. 196.
Hesse, O. (1911). “Das Rontgenkarzinom,” Fortschr. A d. Geb d. Rontgenstrahlen, 17, pp. 82–92.
Inkret, W. C., Meinhold, C., & Taschner, J. (1995). “A Brief History of Radiation,” Los Alamos Science, 23, pp. 116–123. https://fas.org/sgp/othergov/doe/lanl/pubs/00326631.pdf.
Leszczynski, K., & Boyko, S. (1997). “On the Controversies Surrounding the Origins of Radiation Therapy,” Radiotherapy and Oncology, 42(3), pp. 213–217. doi: 10.1016/S0167-8140(97)01940-3
Meinhold, C. (2004). “Lauriston S. Taylor Lecture: The Evolution of Radiation Protection—From Erythema to Genetic Risks to Risks of Cancer To…?” Health Physics, 87(3), pp. 240–248.
National Research Council (NRC) Committee on the Biological Effects of Ionizing Radiation. (1988). Health Risks of Radon and Other Internally Deposited Alpha-Emitters: Beir IV. Washington, DC: National Academies Press (US). doi: 10.17226/1026
Patterson, H. W., & Thomas, R. H. (1973). Accelerator Health Physics. New York: Academic Press.
Rowland, R. E. (1994). Radium in Humans – A Review of US Studies, Argonne National Laboratory Report. doi: 10.2172/10114798
Sansare, K., Khanna, V., & Karjodkar, F. (2011). “Early Victims of X-rays: A Tribute and Current Perception,” Dentomaxillofacial Radiology, 40, pp. 123–125. doi: 10.1259/dmfr/73488299
Scott, N. S. (1897). “X-ray Injuries,” The American X-Ray Journal, 1(3), pp. 59–60.
Stabin, M. (2007). Radiation Protection and Dosimetry—An Introduction to Health Physics. New York: Springer.
Taylor, L. S. (1981). X-ray Measurements and Protection 1913–1964: National Bureau of Standards Special Publication 625. Washington, DC: National Bureau of Standards. https://nvlpubs.nist.gov/nistpubs/Legacy/SP/nbsspecialpublication625.pdf.
Vogin, G., & Foray, N. (2012). “The Law of Bergonié and Tribondeau: A Nice Formula for a First Approximation,” International Journal of Radiation Biology, 89(1), pp. 1–7. doi: 10.3109/09553002.2012.717732.